JACKSONVILLE, Fla. — *This story has been updated to include updated numbers and information from the Department of Children and Families.
Nearly 120,000 Floridians are losing their Medicaid coverage, but not because they're ineligible, according to new numbers from Florida's Department of Children and families sent to First Coast News Friday. A DCF report from April showed that number as 200,000.
Eight members of Congress and more than 50 healthcare advocacy groups are pushing for the governor to pause the Medicaid unwinding process, which is the process where Medicaid eligibility is reviewed.
A report from DCF shows most people are losing their Medicaid coverage because of "procedural issues." DCF's deputy chief of staff says "procedural issues" refers to the person not responding to DCF's attempts to reach them. A community activist as well as a woman First Coast News spoke with whose son remained enrolled in Medicaid believe there are problems on DCF's end.
Because of the COVID-19 public health emergency declaration, people were automatically re-enrolled in Medicaid. Now that's over and, according to DCF's deputy chief of staff, operations have returned to how they were pre-pandemic.
Angela Shenberger's son, Keith, is five years old and has special needs. Because of confusion over the Medicaid unwinding, she feared he would lose his health insurance. If that happened, her son would have to go on her and her husband's health insurance, which Shenberger says would have bumped it up to nearly $1,000 a month.
"I was freaking out because I'm like, if he loses his Medicaid, I don't know what we're gonna do," Shenberger said.
Shenberger's son ended up still receiving Medicaid, but nearly 120,000 Floridians are losing it due to people not responding, according to DCF. DCF's deputy chief of staff says DCF has not experienced system glitches and if someone is not receiving mail or emails they may have opted out.
Shenberger says she did not receive mail she was told to expect.
"No envelope with the yellow stripe came," Shenberger said. "And from what I've heard from a lot of people, they keep saying, 'Oh, we sent it to you, we're gonna send it to you.' Nobody's getting that."
Community Activist Vanessa Brito says people have been experiencing website glitches and have not received mail or emails. Updated numbers from DCF sent to First Coast News Friday show 56 percent of the people losing Medicaid are losing it due to procedural issues. Numbers from a DCF report in April showed that number higher, at 80 percent.
"Imagine you find out at the pharmacy that your EpiPen is now $600 and is no longer covered because you lost coverage," Brito said. "That has always been the fear that people are going to find out when they're actually in the process of either checking into the emergency room, heading to the doctor or picking up a medication."
Brito says many people are now caught in a coverage gap where they may not be able to get health insurance until next year. She explains in order to be referred to Healthcare.gov, you must be determined ineligible for Medicaid; however, she says some people do not know they are determined ineligible and therefore do not apply for coverage within the allotted time.
Brito refers to this January report from the Centers for Medicare and Medicaid Services which states: "Due to the volume of individuals expected to lose Medicaid and CHIP coverage, Medicaid and CHIP agencies may be unable to provide timely information about the termination of coverage and coverage options that would enable consumers to make an informed decision about their coverage options within 60 days. For example, a consumer may need clarity as to whether a loss of Medicaid or CHIP coverage was procedural or due to ineligibility before deciding whether to pursue Marketplace coverage."
DCF's deputy chief of staff says losing coverage counts as a "qualifying life event" for coverage at Healthcare.gov, which can make you eligible for a special enrollment period.
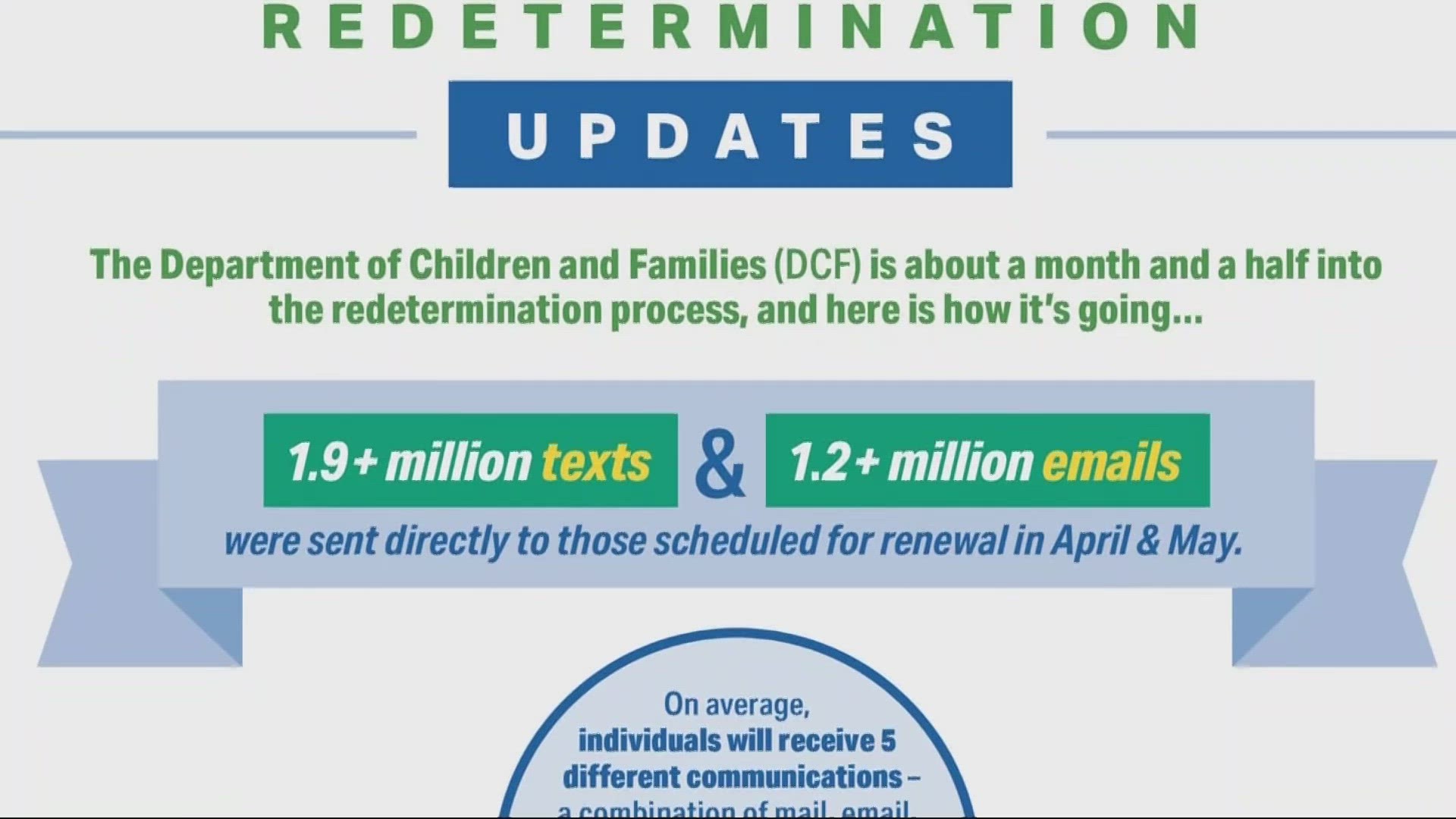
A DCF spokesperson says DCF has a "robust outreach campaign, including up to 13 direct contact attempts to customers who do not submit a timely application." They say outreach efforts have led to a 20 percent increase in their response rate compared to previous redetermination cycles.
Shenberger got a head start on the process and says she was checking her 'My Access' account multiple times a day. Brito says you won't be notified if your account information is incorrect and you must stay on top of it. She says you should go to an office if you cannot access your account or get through on the phone.
Join the First Coast News Facebook group Navigating Florida's Unemployment Maze, where Brito is a moderator, if you have more questions.
The governor's office did not respond to First Coast News's questions about calls to pause the Medicaid unwinding process.