ST. JOHNS COUNTY, Fla. — Firefighters, paramedics, and emergency medical technicians routinely risk their lives to save others.
“We’re used to going in to dangerous situations,” 16-year St. Johns County Fire Rescue veteran Captain Bob Snell said in a recent interview. But most dangers that first responders face are visible to the naked eye. The coronavirus pandemic has added a danger that’s not only relatively unknown, it’s invisible. And emergency staff know that a close encounter with a COVID patient is always just a phone call away.
“It starts with 9-1-1,” Snell explained, as emergency call center staff has been trained to ask questions that can alert responders of a potential coronavirus situation. But that’s just the beginning of how emergency response has abruptly altered in recent months.
“[The crisis] forced us to look at every aspect of what we do, every aspect of how the station operates,” Snell said.
Of course that would mean new equipment and procedures, but also the need for people to train frontline responders and oversee actual operations to ensure consistent adherence to proper measures.
“Folks on the ambulances, on the engines, do a great job of treating the public,” Snell said. “But with our new demands for personal protective equipment, protecting ourselves, decontamination, there was just a lot of stuff that we needed to do to make sure that our people were protected.”
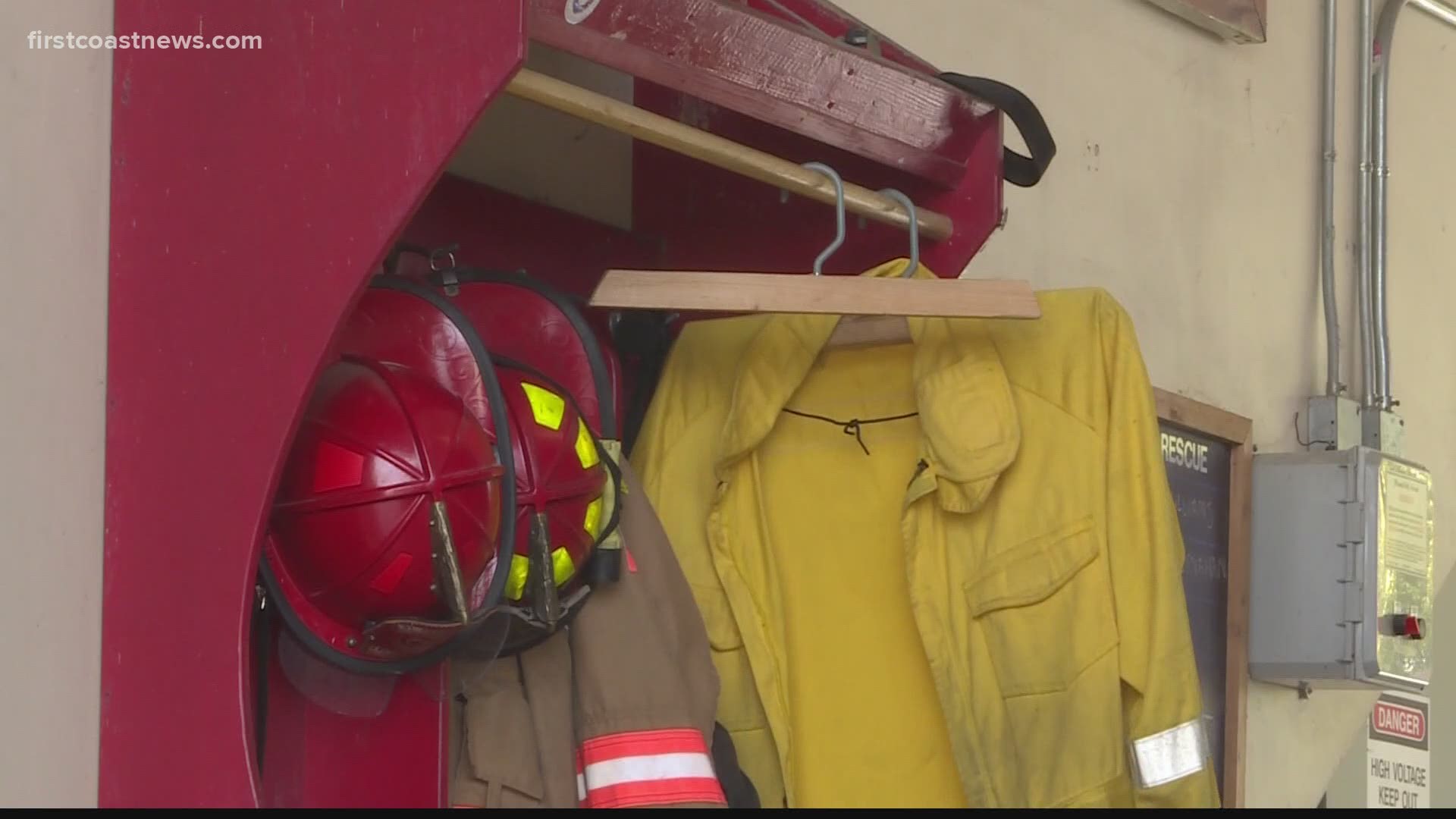
To execute in that capacity, Snell and almost 20 others among more than 300 St. Johns County Fire Rescue personnel were designated infection control officers. They knew that new protocols regarding personnel, equipment, and clothing were crucial to avoid a quick descent into disaster, “to make sure that if they were exposed to a COVID patient, that they didn’t bring it back to the station, didn’t bring it back home with them,” as Snell put it.
Now, if the department suspects that a call might involve a coronavirus case, they don more protective clothing than ever.
“Typically we’d wear gloves, we wear eye protection, but we have never worn masks before, we have never worn gowns before,” Snell began to detail. “The addition of the gown, the addition of the N-95 mask, the routine wearing of eye protection was all something new to us on a routine basis.”
Snell said those extra layers have already proven a challenge, even before the most stifling heat that a Florida summer has to offer.
“It makes it a lot warmer environment, puts a lot of stress on the body.”
If a potential COVID-19 patient requires transportation to a hospital, the interior of the ambulance must be disinfected, including the cab but with particular attention to the back compartment, “our little mobile E.R.,” as Snell described the space.
“It’s not safe for anybody else to ride in the back until we’ve completely made sure that we’ve gotten rid of any traces,” he said. “They need to make sure that they decontaminate everything that the patient has come in contact with.”
To accomplish an adequate decontamination, technicians first wipe down all accessible surfaces and items with antiviral solutions. But that’s not sufficient by itself: the next step is to bring a fogging machine in, a device that emits a visible cleansing vapor, intended to kill any virus cells hiding in the most remote and miniscule orifices. The process, Snell said, adds “a good half-hour, 45 minutes at least” to the time it takes to prepare the vehicle for its next use.
And then there are the first responders themselves, as well as their clothing.
The requirement now is “to immediately go to the shower, take a shower, change their clothes, put on a fresh set of clothes,” Snell said.
That’s not at the end of the shift, it’s at the completion of every COVID-potential call.
“It’s kind of choreographed, even down to that piece of how can they get from the truck to the showers as quickly and directly as possible.”
Even in a communal environment such as a fire station, where shifts are typically 24 hours long and responders have accommodations for food and rest, that frequent need to change clothes is an added stress. Asked how many sets of clothing a responder might go through during one shift, Snell said “It can be quite a few.”
But even brief conversation with these frontline life savers brings a conspicuous revelation: their commitment somehow seems even more intense than ever.
“The drive here was, we weren’t just protecting ourselves as individuals, but protecting the people who are closest to us,” Snell said of the new and developing protocols, a statement encompassing both family and co-workers. But sometimes the people closest to first responders are complete strangers, the very people whose lives the responders are charged with trying to protect and sometimes save.
“A lot of the satisfaction that we get out of our jobs is doing these things that challenge us and that are sometimes dangerous,” Snell said, adding “but ultimately, incredibly rewarding.”
Acknowledging that the new and unprecedented measures might become lasting requirements, Snell was clearly already proud of how first responders – especially his peers in St. Johns County – have adapted and even embraced meeting a new challenge, one that threatens them every day.
“It is a testament to everybody, the courage that everybody’s shown.”